How food affects blood glucose (blood sugar)
Blood glucose naturally rises after you eat. What matters is how high it goes, how fast it rises, and how quickly it returns toward your usual range. Your meal composition, portion size, and even what you do after eating can shape that curve.
What is a “post-meal blood sugar spike”?
After a meal, carbohydrates are broken down into glucose, which enters the bloodstream. The body responds by releasing insulin, helping move glucose into muscles and other tissues. A “spike” usually refers to a larger or faster rise than your body comfortably handles.
Some people notice this as sleepiness, an energy drop later, or stronger cravings. Others feel nothing obvious, which is why a simple framework for steadier meals can be useful.
Why the same meal can affect people differently
Two people can eat the same food and see different glucose responses. Factors include:
- Insulin sensitivity (how effectively your body uses insulin)
- Sleep and stress levels
- Muscle mass and daily movement
- Meal timing and what you ate earlier in the day
- Portion size and food processing (whole vs. refined foods)
Practical, science-based habits to reduce post-meal glucose rises
You do not need perfection. Even small, repeatable changes can make meals “feel” steadier and may support better long-term consistency.
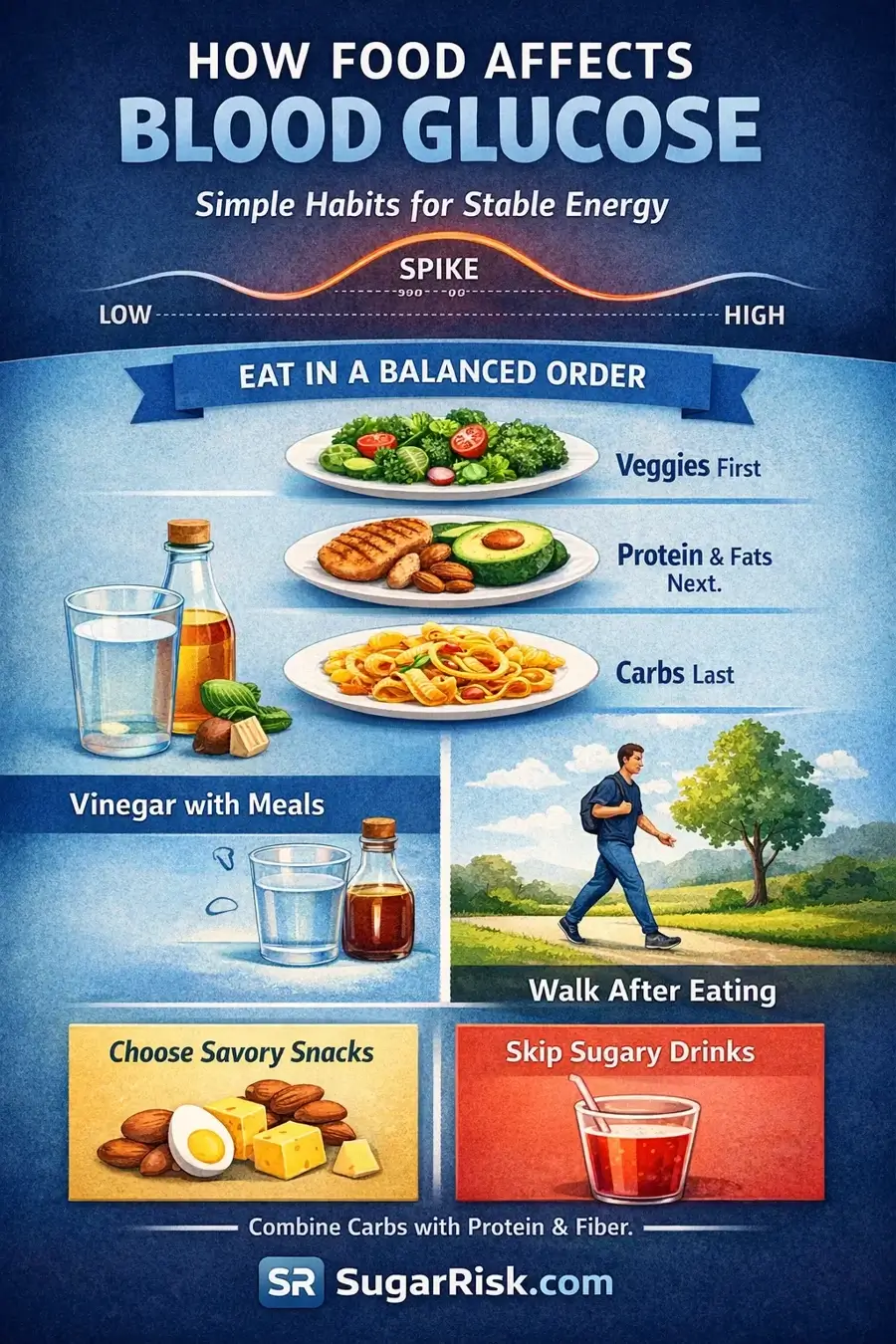
1) Build meals in a balanced sequence
Many people find it helpful to start with fiber-rich foods (like vegetables), then eat protein and fats, and leave refined starches or sweets for last. This approach can slow digestion and reduce how quickly glucose enters the blood.
2) Add a vegetable “starter” (even a small one)
A few bites of vegetables before the main part of the meal can increase fiber early, which may moderate the glucose rise—especially when the meal includes bread, rice, pasta, or dessert.
3) Pay attention to food quality, not only calories
Calories are a useful metric, but they do not describe the full metabolic effect of a food. Meals with more protein, fiber, and less refinement often produce steadier glucose patterns than highly processed, low-fiber options.
4) Choose a protein-centered breakfast for steadier mornings
If your mornings include sweet or refined carbs, consider shifting toward protein plus fiber (for example eggs with vegetables, yogurt with nuts and berries, or a savory bowl with beans). This can support steadier energy and fewer mid-morning cravings.
5) Understand that “natural sugar” is still sugar in the body
Honey, syrups, and refined sugar are metabolically similar in the sense that they can raise glucose. What often matters most is context: whether sugar is eaten alone or as part of a balanced meal.
6) If you want something sweet, pair it with a real meal
Sweets on an empty stomach can produce a sharper rise. Having dessert after a balanced meal can slow digestion and reduce the rapid absorption that drives bigger spikes.
7) Use acidic foods as part of meals
Some people use vinegar-based dressings or small amounts of vinegar diluted in water with meals. As part of a meal pattern (not as a “quick fix”), acidic ingredients may modestly slow the digestion of carbohydrates for certain people.
8) Move a little after eating
Light movement after meals—like a short walk, gentle cycling, or simple bodyweight activity—helps muscles use glucose for energy. This can reduce how much glucose remains in the bloodstream after eating.
9) Prefer savory, protein-based snacks
If you snack, consider options that include protein and healthy fats (nuts, cheese, eggs, hummus, Greek yogurt). These tend to be more stable than sweet snacks eaten alone.
10) Combine carbohydrates with protein, fat, and fiber
Carbs are not “bad” by default. The goal is to avoid eating refined carbs by themselves. Adding protein, fat, and fiber can slow digestion and make the overall glucose response smoother.
A simple “steady plate” you can use anywhere
- Half the plate: vegetables or salad
- Quarter: protein (fish, chicken, eggs, tofu, beans)
- Quarter: carbs (rice, potatoes, pasta, bread) — adjust portion to your goals
- Add: a source of healthy fat (olive oil, nuts, avocado) if appropriate
How to track what works for you
If you like data, you can use your routine measurements (fasting glucose, A1c results, or a glucose log) to see patterns over time. Some people also use a CGM, but it is not required to benefit from the habits above.
If you want a quick reference tool on this site, try: Blood Sugar Checker → or A1c to Average Glucose Converter →.
Related reading
Continue learning: Insulin resistance explained → · How to lower prediabetes risk naturally →
Next step
Want a quick check? Try the Prediabetes Risk Test → or use the Risk Calculator →.